The tragic fate of the people who stop sleeping
Silvano was on a cruise ship when the family curse struck. An elegant 53-year-old with striking red hair who enjoyed wearing a tuxedo at every possible occasion, he tried to present himself with the poise of the film stars he admired. But while on the ship’s dance floor one evening, he was embarrassed to find that his shirt had become drenched in sweat.
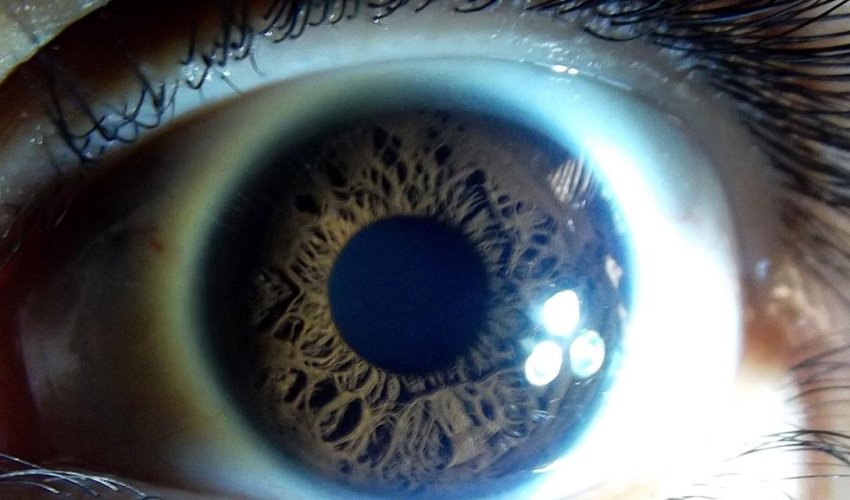
Concerned, he examined himself in a mirror, only to find that his pupils had shrunk to two tiny black pinpricks. It was the same glassy-eyed stare that had afflicted his father and two sisters at the beginning of their mysterious illnesses.
He knew this was just the beginning. Tremors, impotence and constipation could follow. But the most terrifying symptom would be the disappearance of sleep – almost total insomnia for months; a kind of waking coma that ultimately would end in death.
Silvano eventually referred himself to the University of Bologna’s sleep unit for further study, but he was under no illusions about the course of the disease. "He said, ‘I’ll stop sleeping, and within eight or nine months, I’ll be dead,’” one of his doctors, Pietro Cortelli, told me in a phone interview.
"I said ‘how can you be sure?’ He then drew me his genealogical tree from the 18th Century, all by heart.” In each generation, Silvano could name family members who had succumbed to the same fate.
As Silvano had predicted, he died less than a couple of years later, but he left his brain to science in the hope that it might shed some light on the strange disorder that had plagued his family.
What’s going on inside the brains and bodies of people with this strange disease? It’s a mystery that researchers are only now starting to fully understand, and possibly treat with a promising new drug. However, since "Fatal Familial Insomnia” (FFI) involves a genetic legacy that is passed through generations, this research is also raising a difficult and ethically fraught question: if your family’s genes meant you could one day be struck down by the inability to sleep, would you want to be told your fate?
Patient zero
Silvano’s family have mostly remained silent about their struggle with FFI, but about 15 years ago they opened up about their history to the writer DT Max, whose book The Family Who Couldn’t Sleep offers an engrossing portrait of a family living in fear of their own genes. Hunting for "patient zero”, Max found the disease could be traced as far back as a Venetian doctor who fell into a continuous, paralysed torpor during the late 18th Century. Soon after, a nephew named Giuseppe succumbed to a similar fate, and from there, the illness passed through his sons Angelo and Vincenzo to their children and great grandchildren, until it reached Silvano’s father Pietro, who died during World War Two.
Despite this chain of losses, the family tried not to talk about the illness for fear of tempting fate, but that changed in the 1980s when Silvano started developing his symptoms. His niece had married a doctor named Ignazio Roiter, and as a man of science, he persuaded his wife’s uncle to visit Elio Lugaresi’s famous sleep clinic at the University of Bologna, where Cortelli was working.
The Venetian family live in fear of "una notte in bianco" - a sleepless night that might signal the start of their decline (Credit: MahPadilha/Flickr/CC BY 2.0)
Together, they set about solving the mystery of the illness. Although their efforts could do nothing to save Silvano or two other family members who would succumb shortly afterwards, extensive testing eventually found the culprit: a misshapen protein in the brain called a prion, caused by a tiny genetic mutation. For some reason it is only at middle age that the prions begin to proliferate wildly, collecting in pockets that poison the neurons.
The size and shape of a walnut, in Silvano’s brain the thalamus appeared to have been riddled with boring worms
This made it a relative of Creutzfeldt–Jakob disease (CJD) and Mad Cow Disease – two other prion diseases that were garnering serious scientific interest at the time. But whereas CJD leaves the surface of the brain looking like Swiss cheese, Silvano’s condition seems to target parts of the thalamus, at the very centre of the skull. Normally the size and shape of a walnut, the thalamus in Silvano’s brain appeared to have been riddled with boring worms.
After years of further research, the scientists can now explain why damage to this small nub of neural tissue unleashes such a puzzling constellation of symptoms. We know, for instance, that this hub orchestrates all our "autonomic” responses to the environment – things like temperature control, blood pressure, heart rate, and the release of hormones to keep the body ticking over comfortably. When it breaks down, it is as if your central heating is going haywire, your water pipes have sprung a leak, your windows are wide open and your loudspeakers are blaring at full volume – everything is in chaos. Hence the profuse sweating and shrunken pupils, the impotence and the constipation.
Turning off consciousness
This erratic autonomic control could also contribute to the patients’ insomnia: their bodies can’t prepare for a night’s sleep. Where blood pressure typically drops before sleep, theirs would be abnormally high, for instance, giving the sensation that their body is still on high alert. "If the sympathetic nervous system is unbalanced, of course you’ve got insomnia,” says Cortelli, who presented his ideas in a recent issue of Sleep Medicine Reviews.
Compounding these issues, the brain’s rhythms are now in complete disarray. During the night, we normally experience periodic cycles of "rapid eye movement” punctuated by a deeper "slow wave” sleep. During this stage, low-frequency oscillations of electrical activity ripple across the cortex – the gnarled, bark-like tissue on the surface of the brain. This appears to calm down the buzz of coordinated conscious activity you’d normally see when we are awake, while also performing important maintenance work, such as consolidating our memories. And what nub of neural tissue deep in the brain orchestrates those delicate rhythms? The thalamus. Lacking this dimmer switch, the FFI patients are always switched on and can never descend into deep, restorative sleep, says Angelo Gemignani at the University of Pisa, who has demonstrated that people with FFI are missing this important pattern of brain activity.
Without those slow waves, the closest they get to normal sleep is a kind of mindless stupor – not quite asleep, but not quite aware, in which they mindlessly mime their routine daily activities. Cortelli thinks this is a pale remnant of the REM stage that punctuates the deeper stages of sleep; in some ways, it looks like they are acting out dreams. He remembers a woman, Teresa, who would mindlessly mimic the action of combing someone’s hair; she had been a hairdresser before the disease struck.
Slowed decline
One remarkable patient, however, has hinted that there may be some unusual ways to alleviate the misery. A psychologist at Touro College in New York, Joyce Schenkein first came across Daniel not through her work, but through a radio chat line (a precursor to internet forums in the 1990s). "His profile was very clever – he was a brilliant guy, extremely funny,” she says; they ended up having a long-distance friendship. (Daniel’s name has been changed to preserve his family’s privacy.)
In a conversation a few years later, he started to sound confused and vague. "At some point, he said ‘pardon me if I sound incoherent but I haven’t slept for five days,’” says Schenkein. Medical tests revealed he was carrying the FFI mutation. (His mother had apparently known there was some illness in his father’s family, but had decided not to worry her son with the details.) Worse still, it was the form that should progress most rapidly.
Rather than crumbling into despair, his response was to buy a motorhome and travel across the US. "He was an adventurous spirit – he wasn’t just going to sit there and die,” Schenkein says. As the symptoms became more extreme, he employed a driver, and then a nurse, to take over the steering wheel when he was too unwell, she says.
Meanwhile (and sometimes with Schenkein’s advice) Daniel was determined to try as many potential treatments as possible, ranging from vitamin supplements and exercise to improve his general fitness to anaesthetics such as ketamine and nitrous oxide, and sleep medicines like diazepam – anything that would give him a few winks of sleep, even for as short as 15 minutes at a time. He even bought a sensory deprivation tank, having found that even under an anaesthetic, his fragile slumbers could be interrupted by the slightest sound or movement.
Floating in the egg-shaped cocoon while bathed in warm salt water, he found the rest that had proven so elusive, enjoying a blissful four-and-a half hours of solid sleep. Once he awoke, however, he had to face terrifying hallucinations – including a strange uncertainty as to whether he was alive or dead.
Despite these (relative) successes, Daniel still faced regular relapses that became more intense as the disease progressed. "When the symptoms reared themselves, he couldn’t do anything,” says Schenkein. "There were times when he lost the whole day – it takes over your consciousness. He could sit there without the initiative to move; he’d be frozen in time.” Once, he tried electroconvulsive therapy to see if the sharp electric shock could knock him out; it did, but he suffered such bad amnesia afterwards that it seemed a far from ideal solution. After a few years of this struggle, he too finally passed away.
Clearing the debris
Although none of the treatments provided long-term relief, Daniel lived years longer than his diagnosis might have predicted. Schenkein points to recent evidence showing that slow-wave sleep triggers currents of cerebrospinal fluid to wash through the channels between brain cells, carrying away the debris and detritus from the day’s activity, and leaving it clean like the beach after high tide. Perhaps, by alleviating the insomnia, you can encourage this clean-up and forestall the brain’s further disintegration. Together with the Italian neurologist Pasquale Montagna (who had worked on those other cases of fatal familial insomnia), Schenkein wrote up the case study for a medical journal in the hope it may inspire others to look for measures to extend the life of patients with FFI.
"It at least opens the possibility to say that there is something we can do,” says Cortelli – though he emphasises that we can only learn so much from a single case report; it is unclear if similar measures would help any other sufferers.
(Source BBC)
www.ann.az
Similar news
Similar news
Latest news 
More news 



































 Photo
Photo 



 Video
Video 

